Discover ITS
An online tool to enhance your course curriculum in the field of behavioral and mental health service.
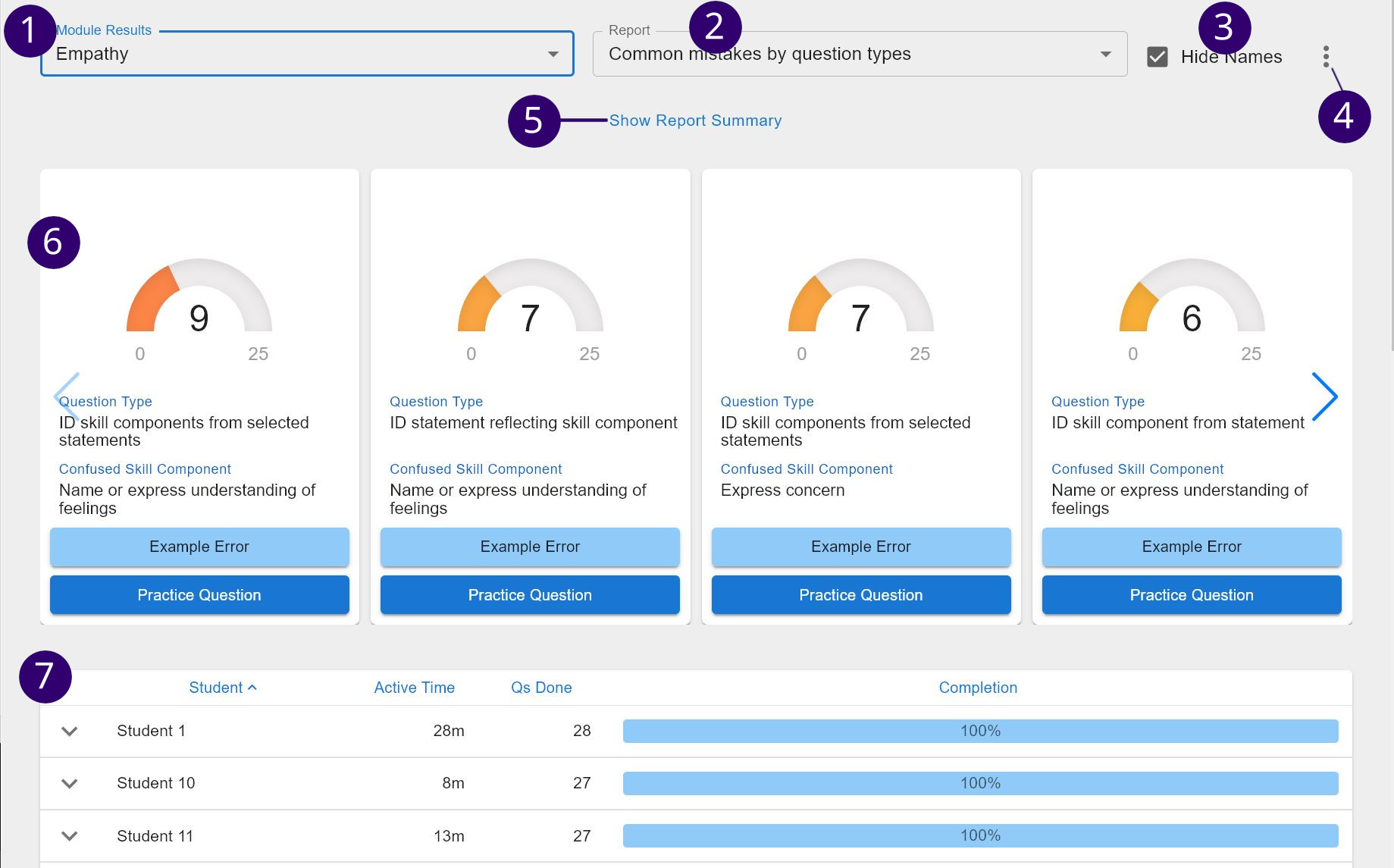
Provide your students with essential practice in a variety of skills, along with tools to analyze their performance.

Learn more about ITS (the Intelligent Tutoring System) and how to include it into your next course below!
The Intelligent Tutoring System (ITS) is an online program designed to teach basic clinical skills relevant to behavioral interventions and other structured psychotherapies. It was developed based on the ITS creators’ own original research, as well as previous research in the fields of learning science, educational technology, machine learning, and knowledge representation. Several studies show that when students are exposed to an intelligent tutoring system as part of their training, they perform as well as students who are trained by seasoned professionals and they demonstrate better problem solving skills and higher self-efficacy in clinical situations.
The ITS utilizes a framework called “productive struggle”, which is a scaffolded learning approach that involves practice with clinical concepts and goes beyond passive reading, listening, or watching. In productive struggle, students are given novel tasks that are challenging; the tasks must be challenging enough that the student learns something new in the process, but not so difficult that the student becomes frustrated and discouraged. Recognizing that students learn at different rates, the ITS is able to adapt to each student’s pace of learning. The program gradually increases in difficulty as the student better understands the topics, keeping an effective level of productive struggle at all times.
Each clinical skill is taught via an interactive, case-based online module. Module options include: therapeutic alliance skills (empathy, reflective listening, cultural responsiveness), session organizational skills (agenda setting, redirection), intervention skills (enhancing motivation, assigning homework, reviewing homework), and suicide risk skills (assessment and management of suicide risk). As an instructor, you have the freedom to choose the modules relevant to the course you are teaching.
See below for more details about each module offered.
Empathy is a core component of the therapeutic alliance. When patients express negative or distressing feelings or experiences, we want to communicate acceptance and concern both verbally and non-verbally. This skill is particularly relevant when we are reviewing distressing symptoms or problems in living, but empathy should be a component throughout the encounter.
Reflection is a core component of the therapeutic alliance. We restate what patients have said on those occasions where we want to highlight their experience, and in particular ensure their awareness of the link between distressing behavioral health symptoms or behavior and a particular life circumstance or problem in living.
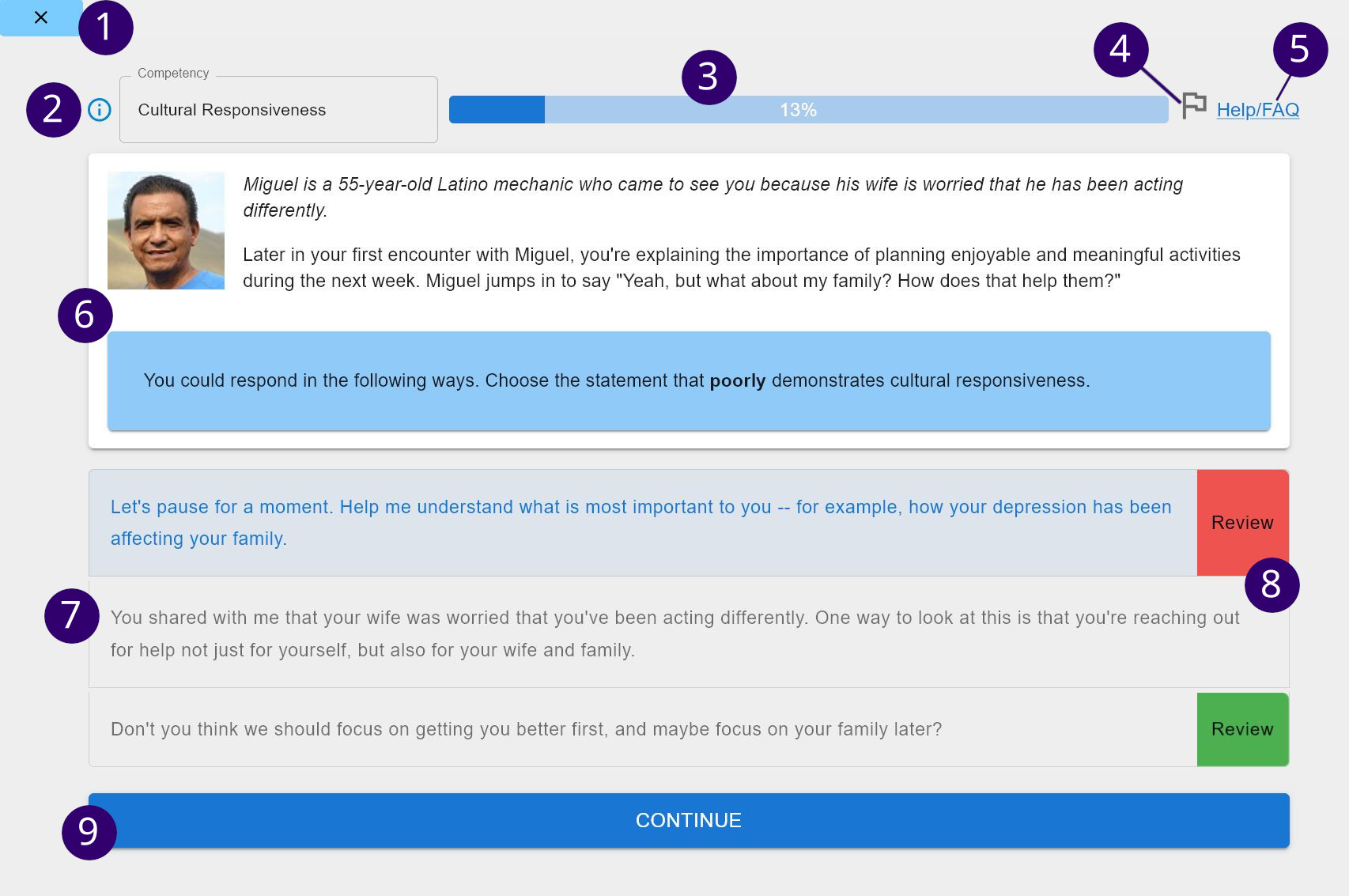
Cultural responsiveness is a core component of the therapeutic alliance. We want to interact with patients and deliver our interventions in a way that is responsive to and congruent with the patient’s cultural identity, context, and preferences. One aspect of cultural responsiveness is recognizing collectivist orientation and the importance of family (and extended family) for many cultures in our conceptualization and treatment, in contrast to the individualistic culture of middle-class White America.
The purpose of agenda-setting at all encounters is to collaboratively structure how time and effort gets spent. Agenda-setting involves patient input in determining ahead of time how to both focus the intervention and ensure that patient priorities are addressed. Setting an agenda at the start of each encounter helps to manage time throughout the encounter. Agendas typically include behavioral health symptom review, homework review, and new goal setting and homework.
At times during our encounters with patients, we may need to redirect them back to the task at hand. We use redirection skills to ensure that patients focus productively on one issue at a time. Good time management starts with agenda-setting at the beginning of an encounter and is maintained by ongoing redirection and focus throughout the encounter.
Patients are often ambivalent about making changes in their lives. We use a variety of strategies to enhance patient motivation and “elicit change talk” to promote positive behavior change. These strategies are particularly helpful before assigning homework in order to ensure patient readiness and agreement.
After providing adequate psychoeducation to the patient about their behavioral health symptoms and about the intervention, we then need to structure the encounter in a way that will be most beneficial to helping the patient learn new skills, all while staying within our time limit. To do this, we focus on setting specific goals, teaching and illustrating therapeutic skills, detailing homework, and anticipating obstacles.
Patients will be more likely to complete their action plans if the provider reviews them at the start of each encounter, discusses the patient’s satisfaction with their efforts, and troubleshoots any obstacles. This discussion of successes helps patients acknowledge and feel good about their accomplishments, even if they are still not functioning as well as they were since their behavioral health symptoms began. Reviewing homework also reinforces for the patient the link between their efforts and improvements in behavioral health symptoms and functioning.
When patients endorse item 9 on the PHQ, or when they report any thoughts of death or suicide, the provider must follow up with a series of questions around thoughts patients may be having in the past month. Risk level range from:
Providers must take the appropriate actions after they determine suicide risk level to be mild to moderate.
Providers must take the appropriate actions after they determine suicide risk level to be high.